ScienceDirect
20 Sep 2023
Highlights
- The complement system plays a vital part in innate immunity.
- Complement plays a role in the development of several ocular diseases.
- Numerous complement-targeting therapies are in development for dry age-related macular degeneration.
- The outer blood–retinal barrier limits access to some therapeutic agents.
- Gene therapies have the potential to provide one-time, localised treatment.
The complement system is involved in the pathogenesis of several ocular diseases, providing a rationale for the investigation of complement-targeting therapeutics for these conditions. Dry age-related macular degeneration, as characterised by geographic atrophy (GA), is currently the most active area of research for complement-targeting therapeutics, with a complement C3 inhibitor approved in the United States earlier this year marking the first approved therapy for GA. This review discusses the role of complement in ocular disease, provides an overview of the complement-targeting agents currently under development for ocular conditions, and reflects on the lessons that can be learned from the preclinical investigations and clinical trials conducted in this field to date.
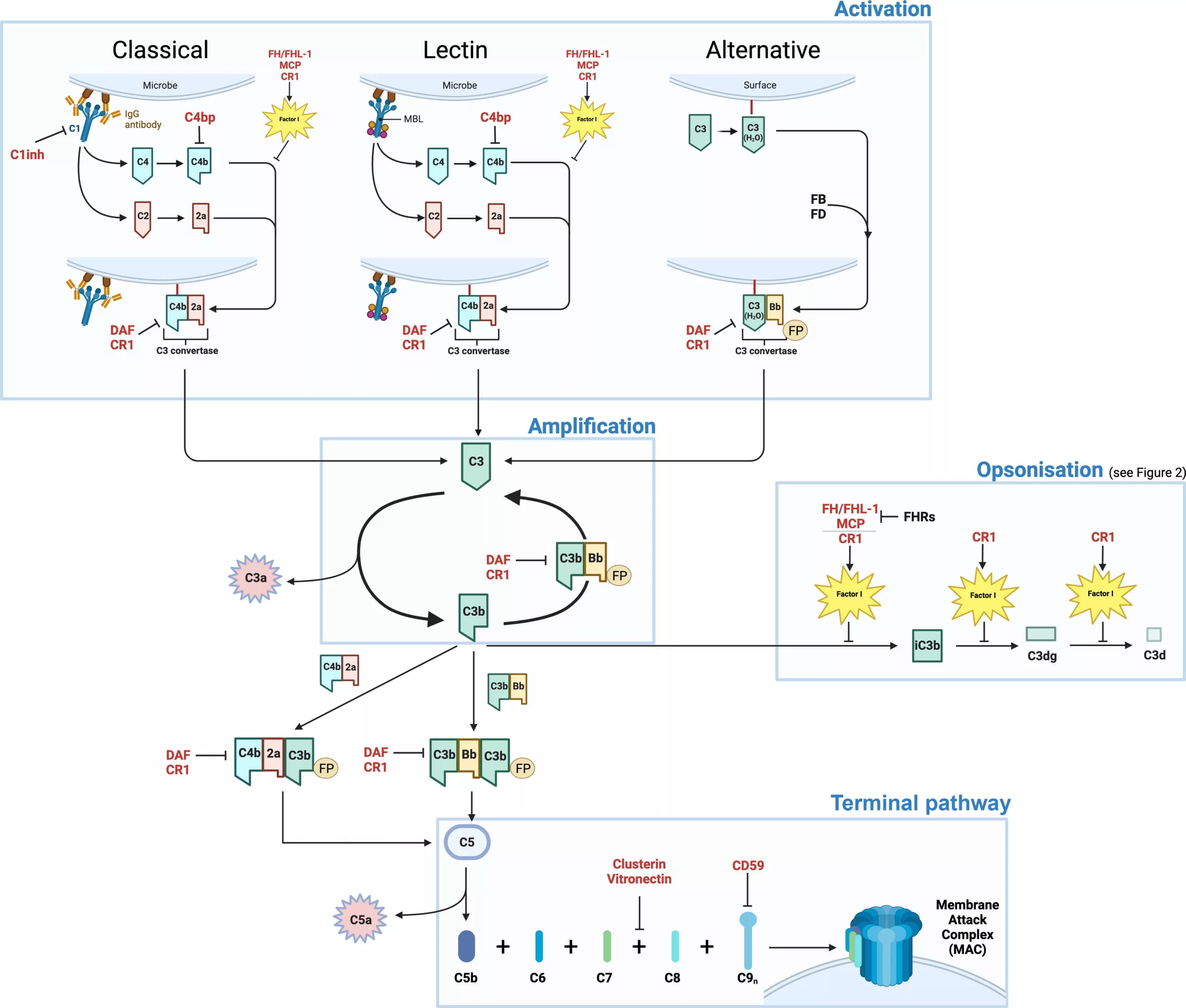
The complement system plays a vital role in innate immunity. It consists of a tightly regulated network of proteins that are activated as a cascade of biological reactions via three different proteolytic pathways: the classical, alternative and lectin pathways (Figure 1).1 The three pathways are each triggered in different ways: the classical pathway is generally activated by the recognition of antigen–antibody complexes by the protein C1q; the lectin pathway by the binding of pattern recognition proteins, such as mannan-binding lectin (MBL), to sugar molecules on the surfaces of pathogens or damaged cells; and the alternative pathway by spontaneous hydrolysis of the C3 thioester bond that results in the formation of a fluid phase convertase capable of cleaving C3 to C3b, which is then deposited on nearby cellular or acellular surfaces.2 While the classical and lectin pathways are triggered by the recognition of ‘foreign’ signals, the alternative pathway of activation remains constitutively active, probing all surfaces with which it comes into contact. In this case, it is up to the host cell or acellular extracellular matrix (ECM) to deactivate deposited complement activators itself and any inability to do so is seen as a danger signal.